A team of researchers led by Prof. Hung-Yuan (Peter) Chi from the Institute of Biochemical Sciences at National Taiwan University has achieved a significant milestone by developing a novel adenovirus-based fluorescence method to monitor DNA repair activity in tumor cells precisely. Notably, it has been successfully applied to tumor cells isolated from ovarian cancer patients, demonstrating its potential to accurately predict clinical responses to medication. This breakthrough contributes significantly to the advancement and realization of precision medicine. The research findings have been published in the prestigious scientific journal Cell Reports Medicine.
Previous studies have established that pathogenic mutations in BRCA1/2 genes result in reduced cellular DNA repair activity, rendering the cells susceptible to Poly(ADP-ribose) polymerase inhibitors (PARPi). Clinical research has shown that tumor cells from different cancer types, including ovarian, breast, pancreatic, and prostate cancer, exhibit a higher proportion of DNA repair deficiencies and respond well to PARPi treatment. However, conventional genetic testing alone is insufficient for the comprehensive and precise identification of eligible patients. This is because, in addition to BRCA1/2 gene mutations, defects in other molecular mechanisms within the cell can also lead to a decrease in DNA repair activity.
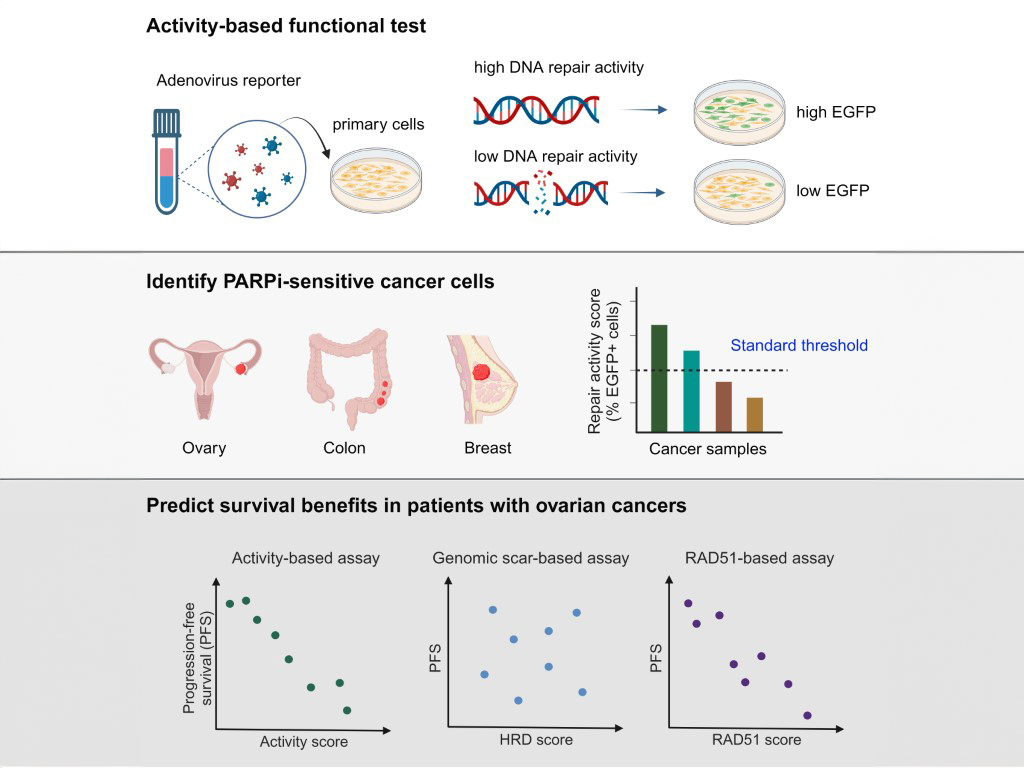
The newly activity-based detection method in this study complements the limitations of genetic testing, providing real-time insights into the DNA repair activity of tumor cells. Furthermore, by analyzing activity values from various types of tumor cells, the research team has identified a standard threshold that can be applied to predict the responsiveness of tumor cells to PARPi in triple-negative breast, ovarian, and colorectal cancer. Notably, in collaboration with the Department of Obstetrics and Gynecology at National Taiwan University Hospital, the research team conducted tests to evaluate the applicability of this detection method to ovarian cancer patients. The results showed that the activity detection method outperforms traditional genetic testing and immunofluorescence staining in accurately predicting the sensitivity of a patient's tumor cells to PARPi. It also effectively distinguishes patients' progression-free survival after frontline treatment. The team’s research revolutionized cancer therapy, showcasing the power of innovation and collaboration in medical science.